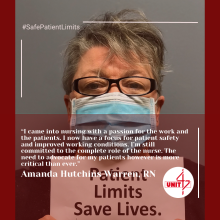
"I came into nursing with a passion for the work and the patients. I now have a focus for patient safety and improved working conditions. I'm still committed to the complete role of the nurse. The need to advocate for my patients however is more critical than ever." - Amanda Hutchins Warren, RN
Amanda Hutchins Warren, RN serves as the Danbury Hospital Nurses Union, Unit 47, AFT Local 5047's representative on Danbury Hospital's staffing committee. She has worked at Danbury Hospital for 27 years. She recently had an opinion article published on ctnewsjunkie.com, calling out Danbury Hospital's fueling of a worsening patient care crisis.
Heeding the Warnings for Connecticut's Patient Care Crisis
As nurses, we knew long before COVID-19 that patients’ healing environments and health professionals’ working conditions had been deteriorating. Then came the pandemic. For nearly three years, we’ve seen unprecedented challenges. We are physically and emotionally exhausted from trying to care for those for whose health and safety we are responsible under impossible conditions.
Five years earlier, we were at the forefront of union-led efforts aimed at one of the root causes of Connecticut’s care crisis: unsafe patient loads. Public Act 15-191, “AN ACT CONCERNING REPORTS OF NURSE STAFFING LEVELS,” went a long way toward improving accountability, but the pandemic has laid bare how much more must be done.
I know this first hand because I serve as Chair of Danbury Hospital’s staffing committee, which itself is the result of the 2015 law. I took on this role in the hope of making a real difference in establishing safe patient limits at our hospital; a shared value among our local union’s membership.
The present climate in our hospital has made this incredibly important task very frustrating. Approximately 600 unsafe staffing reports were filed by my colleagues between September and November of 2022 alone. It is a mountain of evidence demonstrating the critical need for further action.
Most of my work time is devoted to medical-surgical nursing, and the risks and impacts of unsafe staffing cause me sleepless nights. The anxiety is exacerbated by hospital executives and administrators who seem too far removed from the dangers as the patient load rises. They have, at times, been known to send home or cancel nurses voluntarily signing up for additional shifts, even when the ratios are already worse than they should be.
As nurses we know that simply adding just one patient to our workload increases the risk of someone in our care dying by seven percent. Why should family members accept that unnecessary risk for a loved one when hospital administrators have it in their power to help mitigate it?
Then there is the overwhelming concern that unsafe staffing contributes to an already dangerous job for my colleagues and myself. Nationwide, nurses and allied health professionals suffered a nearly 250 percent increase in injuries and illnesses on the job in 2020.
The pandemic has also brought on a disturbing rise in incidents of workplace violence against caregivers. Unsafe patient loads only add to our vulnerability.
Current Connecticut law requires hospital operators to submit staffing plans to the state’s health department. Yet health chain administrators are failing - and in some cases, refusing - to abide by their own blueprints for achieving safe patient limits. That’s why we need bold action that goes beyond aspirational goals and lofty intentions.
Thankfully some leaders in our state and national unions have assessed and compiled some best practices in order to provide practical policy proposals. AFT’s Healthcare Staffing Shortage Task Force recently released comprehensive recommendations that health chain executives should embrace, and state legislators must codify into law.
Many are aimed at what should be an objective that is shared by hospital administrators - to retain experienced veterans and recruit a workforce for the next generation. A national poll earlier this year found nearly 1 in 4 nurses and allied health professionals likely to leave the profession, threatening to further escalate the patient care crisis. The report also encourages the kind of local solution-driven unionism my colleagues and I have been engaged in throughout the pandemic.
We strive to secure more improvements in working conditions amid the care crisis through collective bargaining negotiations with Nuvance Health executives. Going forward however, a holistic approach is needed.
Not all employers are responsive to their workforce - in our case, 600 incidents of unsafe staffing in three months call into question the commitment Nuvance has to their staff and the patients in their care. Not all care workers across the country have a voice on the job - since many hospitals do not have a union, and therefore have little recourse for addressing dangerous conditions.
Some states have legislative initiatives aimed at unsafe conditions that go well beyond the current Connecticut statutes. One such California law has demonstrated real results - in polling among nurses and health professionals, they credited its specific staff-to-patient ratio requirements for both improved retention and quality of care.
So, what are we waiting for here in Connecticut now that we are clearly in a statewide “code blue” patient care crisis? We have given health chain executives and our elected officials the diagnosis. Thanks to our union, a prescription for recovery is in the works. It is now time for action